Top 5 Anti-Inflammatory Supplements for Crohn's and Colitis
May 19, 2025

In this article, we'll explore the five most promising anti-inflammatory supplements for IBD, based on current scientific evidence. We'll also discuss how technology can help you integrate these supplements into your overall IBD management plan.
The Inflammation Connection in IBD
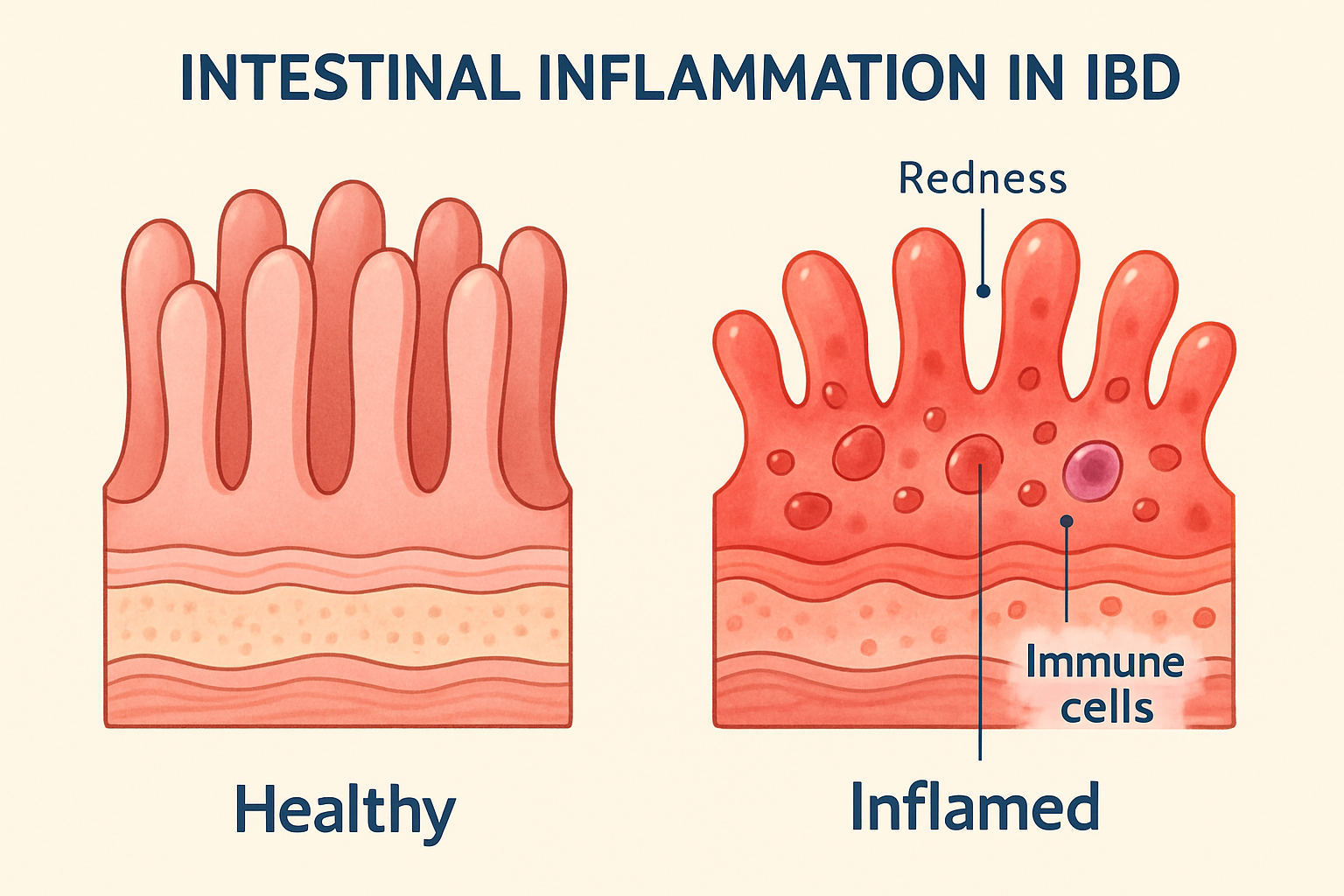
Inflammation causes the microvilli to become inflammed, shorten, and produce less enzymes to break down food. This leads to intestinal permeability which can lead to immune responses.
Before diving into specific supplements, it's important to understand why targeting inflammation matters. In IBD, the immune system mistakenly attacks the digestive tract, triggering chronic inflammation that damages the intestinal lining. This inflammation is responsible for the hallmark symptoms of IBD: abdominal pain, diarrhea, fatigue, and weight loss.
While medications work to suppress this inflammatory response, certain dietary supplements may offer additional support by:
- Directly inhibiting inflammatory pathways
- Supporting the gut microbiome
- Strengthening the intestinal barrier
- Reducing oxidative stress
Important Note: Supplements can reduce inflammation, but they cannot fix a diet that is actively harming you. Most experts agree that removing inflammatory triggers (via AIP, GAPS, Mediterranean, or SCD) is the first step to healing. Supplements are the second step.
Let's explore the top five supplements that show the most promise for IBD patients. As you read, note how most of the supplements below are food based. Food is medicine!
1. Curcumin (from Turmeric)

Forms of Curcumin include raw root, powder spice, and capsule supplements.
Diet alignment:
✅ AIP (note: black pepper is not aligned with AIP principles)
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: Curcumin is powerful, but did you know Turmeric is a staple in our Golden Scrambled Eggs recipe? Getting nutrients from whole foods is often more bioavailable than pills.
What it is: Curcumin is the active compound in turmeric, a bright yellow spice used in many cuisines, particularly Indian food.
How it helps: Curcumin has powerful anti-inflammatory and antioxidant properties. Research shows it can help reduce inflammation in ulcerative colitis specifically by:
- Inhibiting inflammatory pathways like NF-κB
- Reducing the production of inflammatory cytokines
- Protecting the intestinal barrier
The evidence: Multiple clinical trials have shown that curcumin, when used alongside conventional medications like mesalamine, can help induce and maintain remission in patients with mild to moderate ulcerative colitis. A meta-analysis found that curcumin significantly improved clinical remission rates compared to placebo.
Typical dosage: 1-3 grams daily, often divided into multiple doses.
Important considerations: Curcumin has poor bioavailability, meaning your body doesn't absorb it well. Look for supplements that include black pepper extract (piperine) or are formulated for enhanced absorption. The evidence is stronger for ulcerative colitis than for Crohn's disease. If you eat turmeric in your meals, add a pinch of pepper to significantly increase it's benefits.

Enjoying this article?
Every Sunday get new blog articles, recipes, and tips from Chef Kay on how to thrive, one meal at a time.
2. Omega-3 Fatty Acids (Fish Oil)

Sources of Omega-3 Fatty Acids include fish, nuts, seeds, capsule supplements.
Diet alignment:
✅ AIP
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: Supplements are efficient, but our Lemon Herb Baked Salmon delivers a massive dose of Omega-3s in their most bioavailable phospholipid form. Plus, you get the added benefit of high-quality protein without the "fish burps" common with cheap pills.
What they are: Omega-3 fatty acids, particularly EPA and DHA, are essential fats found primarily in fatty fish like salmon, mackerel, and sardines.
How they help: Omega-3s have natural anti-inflammatory properties that may benefit IBD patients by:
- Producing anti-inflammatory compounds called resolvins and protectins
- Reducing pro-inflammatory cytokines
- Improving the gut microbiome composition
The evidence: Research on omega-3s for IBD shows mixed but promising results. Some studies indicate they may help reduce inflammation and improve symptoms in both Crohn's disease and ulcerative colitis. DHA specifically may have protective effects against Crohn's disease development.
Typical dosage: 1-2 grams of combined EPA and DHA daily.
Important considerations: Quality matters with fish oil supplements. Look for products that have been tested for purity and are free from contaminants like mercury. Take with meals containing fat for better absorption.
Here are the Fish Oil products that I use:
- Carlson - Cod Liver Oil, 1100 mg Unflavored, 250 mL (8.4 Fl Oz)
- Carlson - Maximum Omega 2000 (Lemon flavor), 90 soft gels
These are SCD, GAPS, Paleo AIP, and Mediterranean allowed.
3. Vitamin D

Sources of Vitamin D pictured include supplements, milk, salmon, and eggs.
Diet alignment:
✅ AIP
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: While sunshine is the gold standard, egg yolks are one of the few potent dietary sources of Vitamin D. Our GAPS Egg Yolk Drop Bone Broth pairs this nutrient with healthy fats in the yolk, which are strictly required for your body to actually absorb Vitamin D.
What it is: Vitamin D is a fat-soluble vitamin that functions more like a hormone in the body. While we can produce it through sun exposure, many people with IBD are deficient.
How it helps: Vitamin D plays a crucial role in immune function and inflammation regulation by:
- Modulating immune responses
- Reducing inflammatory cytokines
- Potentially improving gut barrier function
- Supporting beneficial gut bacteria
The evidence: There's a well-established link between vitamin D deficiency and IBD. Studies show that maintaining adequate vitamin D levels correlates with less active disease, fewer flares, and better outcomes with biologic therapies. Low vitamin D levels are associated with increased disease severity and relapse risk.
Typical dosage: Highly individualized based on current levels. Your doctor should test your vitamin D levels and recommend an appropriate dosage.
Important considerations: Vitamin D supplementation is often recommended for all IBD patients due to the high prevalence of deficiency and its role in bone health, which can be compromised in IBD.
Here's the Vitamin D that I use:
It is SCD, GAPS, Paleo AIP, and Mediterranean allowed.
Confused about which ingredients are safe?
Taking supplements while eating the wrong food is like bailing water out of a sinking boat. Stop the leak first.
Meadow Mentor acts as your personal chef to help you navigate therapeutic diets (AIP, GAPS, Mediterranean, and SCD) that lower inflammation naturally.
4. Probiotics
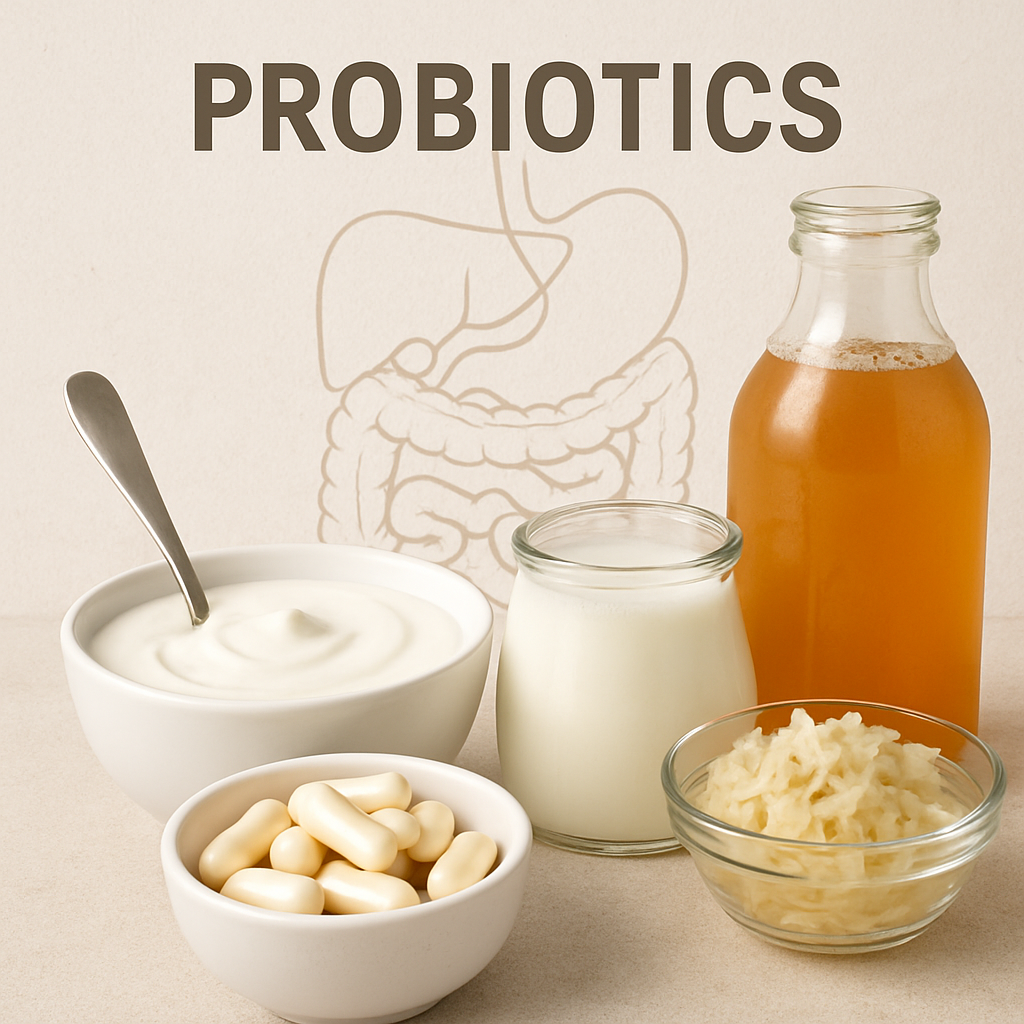
Probiotics pictured include yogurt, capsule supplements, milk kefir, kombucha, and sauerkraut.
Diet alignment:
✅ AIP
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: Most store-bought probiotic pills die before they reach your colon. The live cultures in our SCD-Aligned 24-Hour Fermented Yogurt are cultivated to be trillions of times stronger than standard yogurt, repopulating your gut microbiome with every spoonful.
What they are: Probiotics are beneficial live bacteria that can provide health benefits when consumed in adequate amounts.
How they help: Probiotics may benefit IBD patients by:
- Restoring balance to the gut microbiome
- Strengthening the intestinal barrier
- Modulating immune responses
- Reducing inflammation
The evidence: The effectiveness of probiotics in IBD depends on the specific strain and the type of IBD. Certain strains, like E. coli Nissle 1917 and the multi-strain formulation VSL#3, have shown promise for inducing and maintaining remission in ulcerative colitis. The evidence for Crohn's disease is less compelling.
Typical dosage: Varies by product and strain. Follow package directions or your healthcare provider's recommendations.
Important considerations: Not all probiotics are created equal. Strain specificity matters greatly in IBD. Consult with your healthcare provider about which strains might be most beneficial for your specific condition.
Here's the yogurt starter that I use:
It is SCD and GAPS allowed if you use this as a starter and follow the diet guidelines for making homemade yogurt.
5. Ginger

Forms of Ginger include raw root, powder spice, and capsule supplements.
Diet alignment:
✅ AIP
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: Ginger capsules are great for motility, but cooking with fresh ginger activates digestion immediately through aroma and taste. Our Chicken Ginger Meatballs use fresh grated ginger to help break down the protein proteins for you, making the meal incredibly gentle on a sensitive stomach.
What it is: Ginger is a flowering plant whose rhizome (root) is widely used as a spice and traditional remedy.
How it helps: Ginger contains bioactive compounds with anti-inflammatory and antioxidant properties that may help IBD patients by:
- Inhibiting inflammatory pathways like COX-2 and NF-κB
- Reducing pro-inflammatory cytokines
- Potentially improving gut microbiota diversity
The evidence: While human clinical trials are limited, preclinical studies show promising results. Ginger and its compounds have been shown to reduce inflammation in animal models of colitis. Recent research identified a compound in ginger (furanodienone) that selectively binds to a nuclear receptor involved in IBD, reducing inflammation.
Typical dosage: Up to 2 grams daily.
Important considerations: Ginger is generally well-tolerated but may have blood-thinning effects at higher doses. Human studies on ginger for IBD are still emerging, so consider it a complementary approach rather than a primary treatment.
Bonus: Glutamine

Glutamine is available as powder, capsules, and naturally in protein-rich foods.
Diet alignment:
✅ AIP
✅ GAPS
✅ Mediterranean
✅ SCD
Food source: L-Glutamine powders are popular for sealing the gut lining, but this amino acid was originally discovered in bone broth. Our Ground Beef Sweet Potato Stew provides a rich, natural source of glutamine that is warm, soothing, and instantly absorbed by inflamed tissue.
What it is: Glutamine is the most abundant amino acid in the body and plays a crucial role in intestinal health. It serves as a primary fuel source for the cells lining the intestinal tract.
How it helps: Glutamine may benefit IBD patients by:
- Supporting intestinal barrier function and repair
- Reducing intestinal permeability ("leaky gut")
- Decreasing pro-inflammatory cytokine production
- Promoting healing of the intestinal lining
The evidence: Research on glutamine for IBD shows some promising results, particularly for intestinal permeability issues. Studies indicate that glutamine supplementation may help maintain remission in some IBD patients by strengthening the intestinal barrier. However, clinical trials specifically for Crohn's disease and ulcerative colitis have shown mixed results, with some studies showing benefits while others show limited effects.
Typical dosage: 5-10 grams daily, often divided into multiple doses.
Important considerations: Glutamine is generally well-tolerated, but should be used with caution in patients with liver or kidney disease. It's best taken on an empty stomach or between meals for optimal absorption. While glutamine plays a crucial role in intestinal health, more large-scale clinical trials are needed to fully establish its efficacy specifically for IBD management.
Author Note: I have taken Glutamine off and on for many years to help with my Crohn's disease strictures. It's an essential supplement for me to enjoy a wider diet. I think of it as making the scar tissue more flexible and food is less likely to get blocked in my intestines.
Here are some options for purchasing Glutamine:
- THORNE L-Glutamine Powder - 17.8 Oz - Excellent quality
- Doctors Best Pure L-Glutamine Powder - 10.6 Oz - High quality, value price
- BulkSupplements.com L-Glutamine Powder - 500g (1.1 lbs) - Bulk amount
It's one of those supplements that appears to be easy enough to make that nearly any brand I've tried has been good quality. Don't over think who you buy from as long as the price is right for you. It is SCD, GAPS, Paleo AIP, and Mediterranean allowed.
The Challenges of Supplement Management in IBD
While these supplements show promise, incorporating them into your IBD management plan comes with challenges:
- Information overload: Sorting through conflicting information about supplements can be overwhelming.
- Tracking consistency: It's difficult to maintain a consistent supplement regimen, especially during flares.
- Interactions: Some supplements may interact with IBD medications or be contraindicated during certain disease states.
- Quality concerns: The supplement industry isn't as strictly regulated as pharmaceuticals, making quality variable.
- Personalization: What works for one person with IBD may not work for another.
How Technology Can Help: Meadow Mentor's Approach

Meadow Mentor allows you to see a wealth of information for each meal you log.
Meadow Mentor's app features are specifically designed to help IBD patients navigate these challenges:
- Chef Kay Q&A: Our AI agent Chef Kay can give you evidence-based answers about supplements, potential interactions with your medications, and how they fit into therapeutic diets like the Specific Carbohydrate Diet (SCD), GAPS, Mediterranean, or Paleo AIP.
- Meal Adaptation: Ask Chef Kay how to incorporate beneficial ingredients like turmeric or ginger into your daily meals in ways that are aligned with your therapeutic diet.
- Ingredient Label Analysis: Ask Chef Kay to analyze your photos of supplement labels to check for hidden ingredients that might trigger symptoms or interfere with your therapeutic diet.
Meadow Mentor acts as your personal chef to help you navigate therapeutic diets (AIP, GAPS, Mediterranean, and SCD) that lower inflammation naturally.
Conclusion: A Balanced Approach to IBD Management
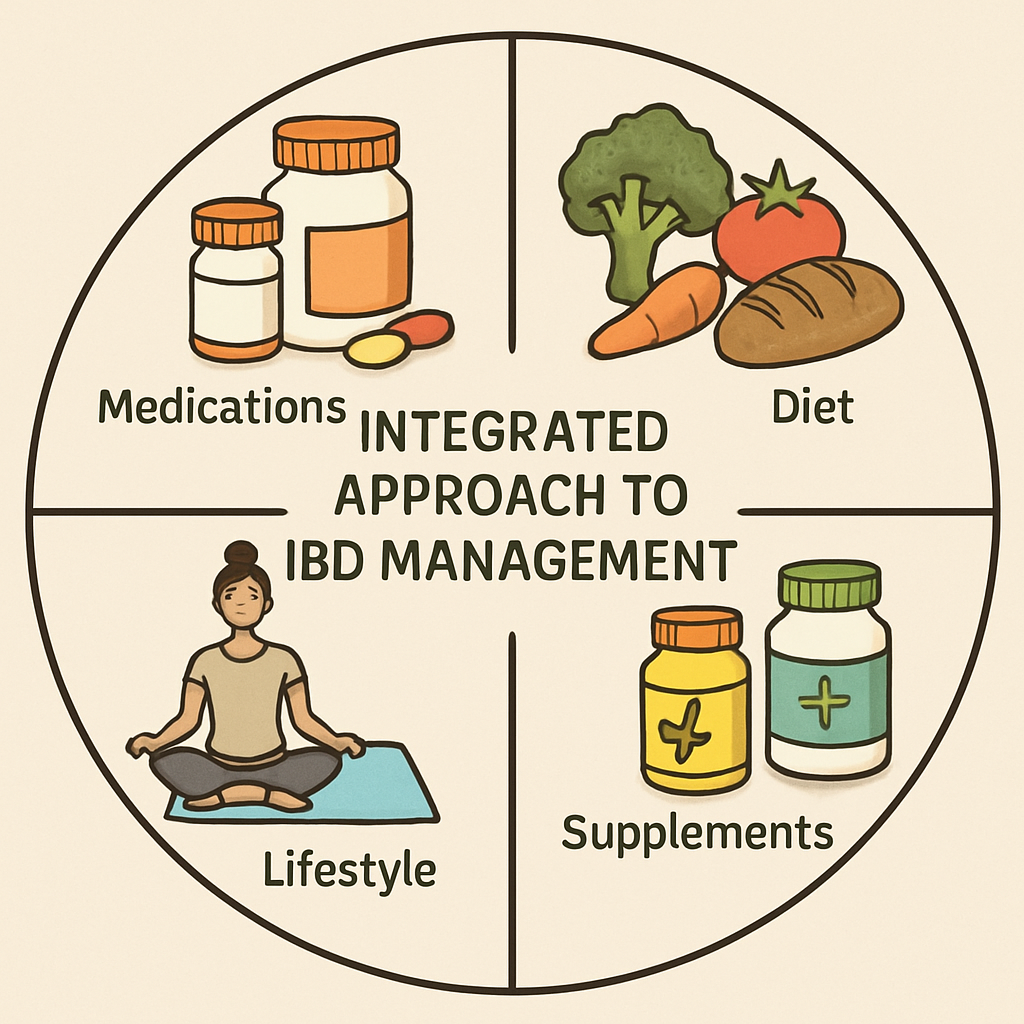
While the supplements discussed in this article show promise for managing inflammation in IBD, they should be viewed as complementary to conventional medical treatment, not replacements. The most effective approach to IBD management typically combines:
- Conventional medications prescribed by your healthcare team
- Appropriate therapeutic diets tailored to your specific condition
- Evidence-based supplements that target inflammation
- Lifestyle modifications like stress management and adequate sleep
By taking a holistic approach and leveraging technology to simplify the complex task of managing all these elements, you can work toward better control of inflammation and improved quality of life with IBD.
Next Step: The Anti-Inflammatory Diet
- Learn about anti-inflammatory diets for gut health
- View our extensive recipes for AIP, GAPS, Mediterranean, and SCD
---
Medical Disclaimer: The information provided in this article is for educational purposes only and should not be considered medical advice. Always consult with your healthcare provider before starting any new supplement regimen, especially if you have IBD or other chronic health conditions. Your doctor can help determine which supplements are appropriate for your specific situation and can monitor for potential interactions with medications or adverse effects.
Note: As an Amazon Associate, I earn from qualifying purchases.

About Reid Kimball
Founder & Builder
Reid has been navigating life with Crohn’s Disease for over 20 years. After discovering the transformative power of the Specific Carbohydrate Diet (SCD) and GAPS, he went from overwhelmed to thriving. He knows how heavy the mental load of meal planning can be. Reid built Meadow Mentor to be the "in-home chef" he wished he had when first diagnosed: a tool to help you navigate therapeutic diets with clarity, confidence, and joy.
